Psychiatry Soap Note Template
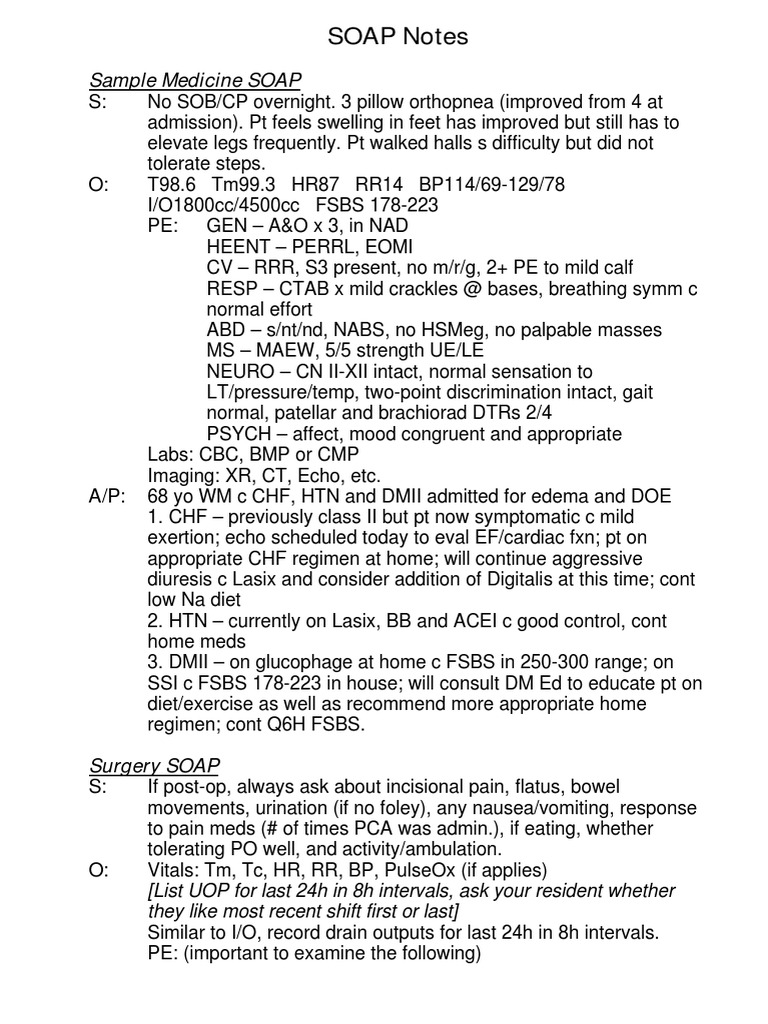
Psychiatry Soap Note Template - Approximately 49 views in the last month. Web comprehensive psychiatric examination. Gait and station / muscle strength and tone: Web in psychiatry, we often document a patient’s current condition and progress in treatment with soap notes. Web mental status examination. She was first hospitalized in her twenties. Depressive symptoms have improved but he still feels. Web mental health professionals can use soap note templates for anxiety and depression for example to ensure they are effectively documenting the essential. Save time with our amazing tool Web initial psychiatric soap note template there are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note.
Psychiatry Soap Note Template
[text name=patientname default=] patient date. Approximately 49 views in the last month. 5+ psychiatric soap note examples; One or more chronic illnesses with. [date name=date default=07/16/2022] patient name:
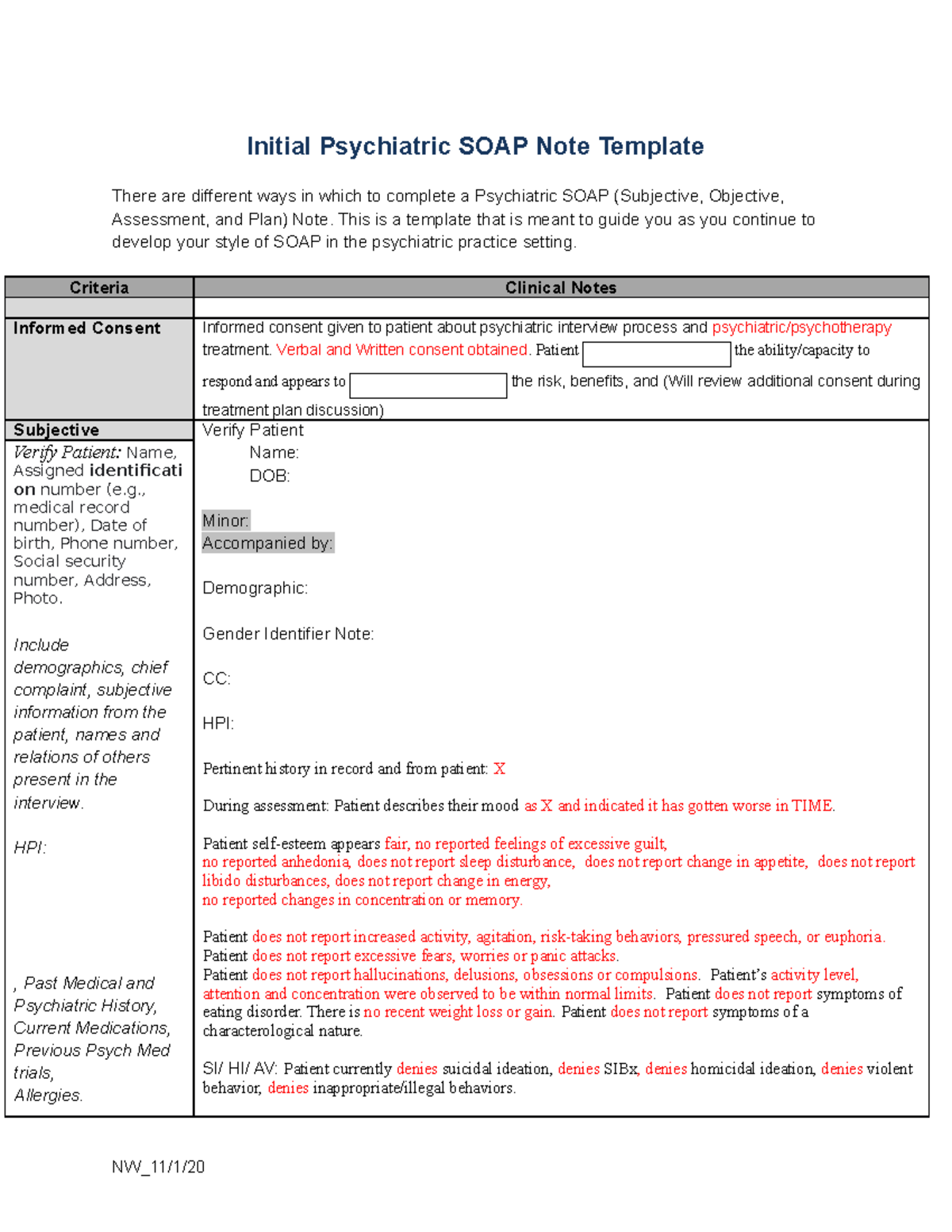
NU646 Initial Psychiatric SOAP Note Template Initial Psychiatric SOAP
Web mental health professionals can use soap note templates for anxiety and depression for example to ensure they are effectively documenting the essential. One or more chronic illnesses with. Chief complaint a statement in “quotes” describing what the patient presents for today: Web high (99215)= psychiatric illness with potential threat to self or others, drug therapy requiring intensive monitoring for.
Psychiatric Soap Note Template
Jan has been hospitalized on a number of occasions. Web by taking typed or handwritten notes according to each category of soap, you can better track and organise your patient care in a standardised manner. As you know, soap stands for the areas of documentation that are. [date name=date default=07/16/2022] patient name: Approximately 49 views in the last month.
29+ Psychiatric Soap Note Example Pics Nalo
Web here’s how to write soap notes. Web initial psychiatric soap note template there are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. She was first hospitalized in her twenties. Save time with our amazing tool As you know, soap stands for the areas of documentation that are.
FREE 9+ Sample SOAP Note Templates in PDF MS Word
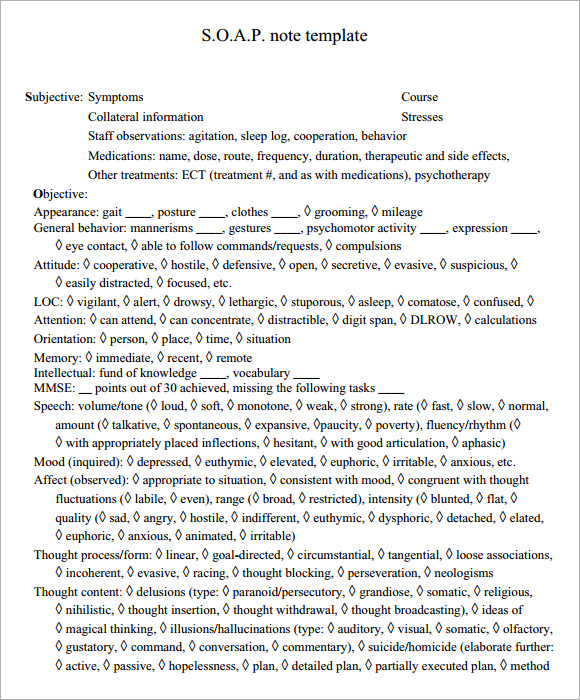
Web comprehensive psychiatric examination. Web in psychiatry, we often document a patient’s current condition and progress in treatment with soap notes. Depressive symptoms have improved but he still feels. Jan has been hospitalized on a number of occasions. Web mental health professionals can use soap note templates for anxiety and depression for example to ensure they are effectively documenting the.
6+ Soap Note Templates Free Word Documents Download Free & Premium
Web in psychiatry, we often document a patient’s current condition and progress in treatment with soap notes. Web comprehensive psychiatric examination. Web mental status examination. Jan has been hospitalized on a number of occasions. Ad fast, easy & secure.
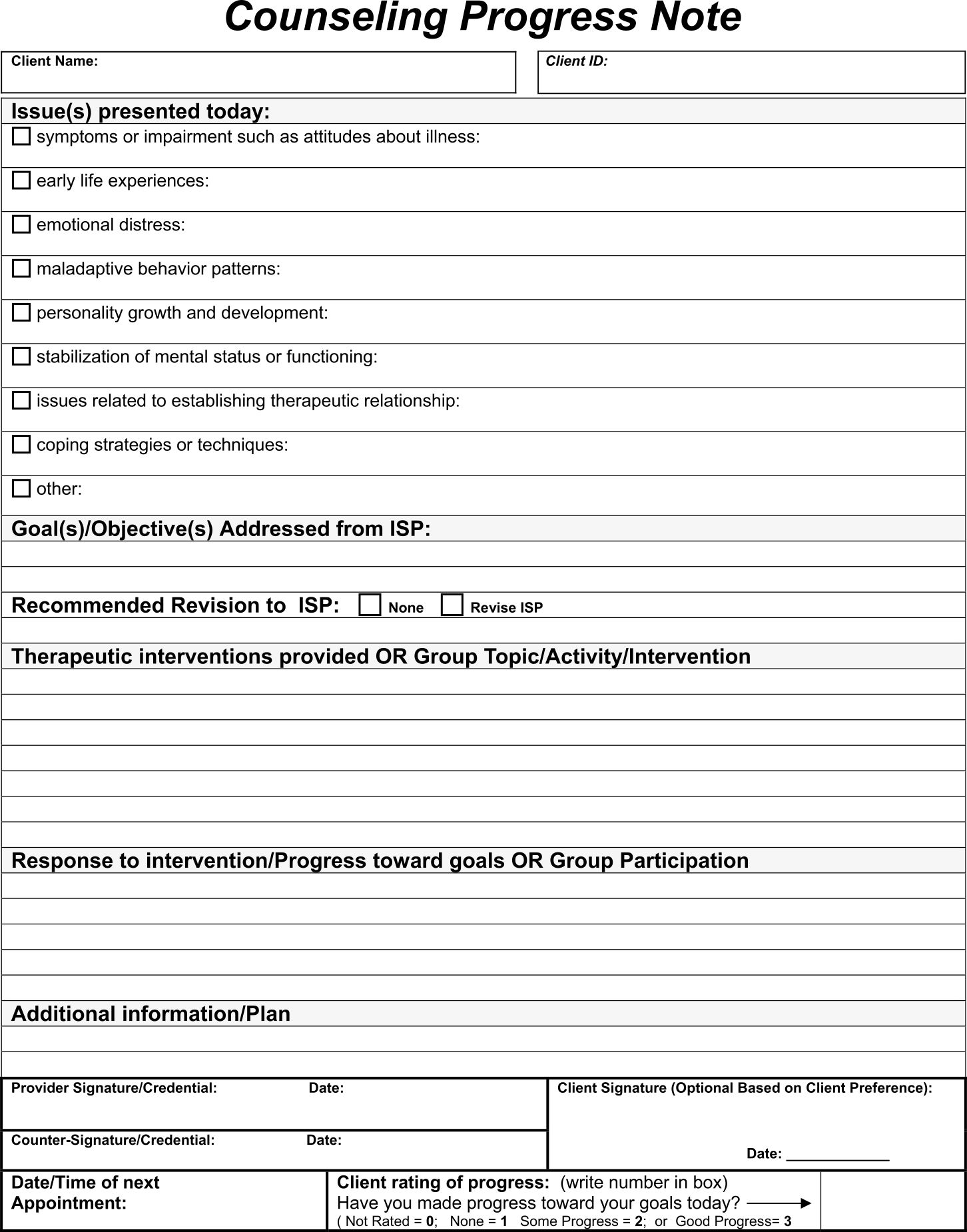
soap note template counseling Google Search Notes Template, Report
One or more chronic illnesses with. Web pmhnp long note. Web mental health professionals can use soap note templates for anxiety and depression for example to ensure they are effectively documenting the essential. [text name=patientname default=] patient date. Web initial psychiatric soap note template there are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan).
Printable Counseling Case Notes Template Printable Templates
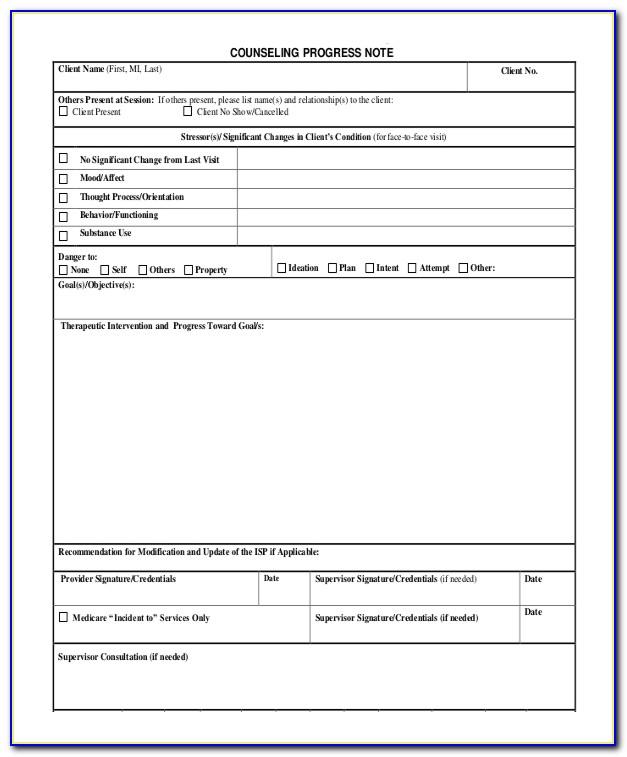
Web soap notes, are a specific format used for writing a progress note.this packet of 8 professionally created soap notes and progress notes can be downloaded and. Ad fast, easy & secure. Web by taking typed or handwritten notes according to each category of soap, you can better track and organise your patient care in a standardised manner. Web past.
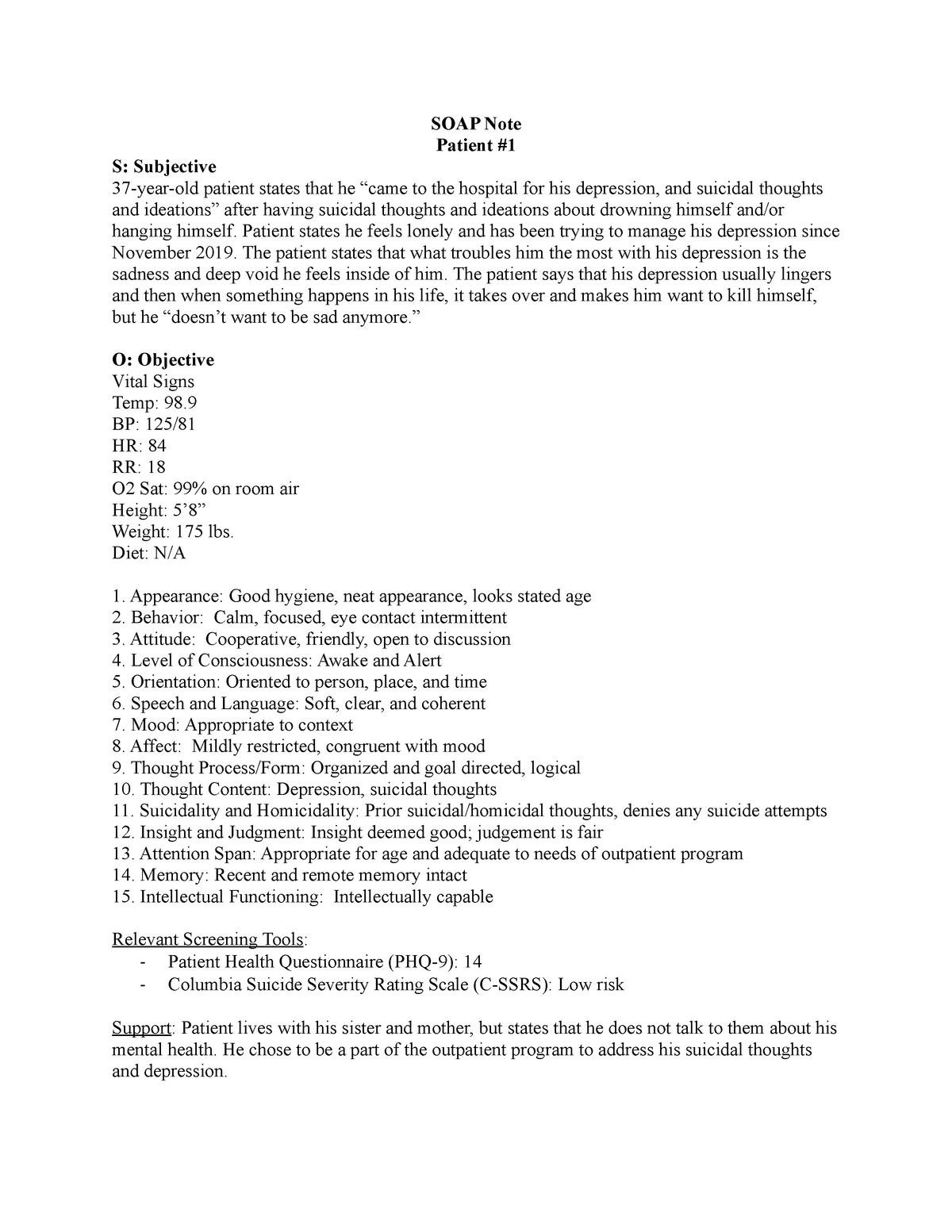
SOAP Note SOAP Notes for Psych SOAP Note Patient S Subjective 37
Web mental health professionals can use soap note templates for anxiety and depression for example to ensure they are effectively documenting the essential. [date name=date default=07/16/2022] patient name: Chief complaint a statement in “quotes” describing what the patient presents for today: Web mental status examination. Web comprehensive psychiatric examination.
Pin on SOAP NOTES
Web high (99215)= psychiatric illness with potential threat to self or others, drug therapy requiring intensive monitoring for toxicity; Nw_11/1/20 criteria clinical notes informed consent. Web initial psychiatric soap note template there are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Depressive symptoms have improved but he still feels. Web past psychiatric history.
Web pmhnp long note. Web in this post, we will review what soap notes are, how to write a soap note, tips for effective soap notes, and a template you can use for your soap notes. Web past psychiatric history : Web initial psychiatric soap note template there are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Web in psychiatry, we often document a patient’s current condition and progress in treatment with soap notes. Jan has been hospitalized on a number of occasions. [date name=date default=07/16/2022] patient name: [text name=patientname default=] patient date. Web mental status examination. Web soap notes, are a specific format used for writing a progress note.this packet of 8 professionally created soap notes and progress notes can be downloaded and. Web comprehensive psychiatric soap notedate: Web this is a template that is meant to guide you as you continue to develop your style of soap in the psychiatric practice setting. Ad fast, easy & secure. Web by taking typed or handwritten notes according to each category of soap, you can better track and organise your patient care in a standardised manner. One or more chronic illnesses with. She was first hospitalized in her twenties. Chief complaint a statement in “quotes” describing what the patient presents for today: 5+ psychiatric soap note examples; Nw_11/1/20 criteria clinical notes informed consent. Approximately 49 views in the last month.